Burn Injuries in Horses
Click here to read the complete article
By Heather Smith Thomas
Barn fires are probably the most common cause of burn injuries in horses, but they may also be burned by lightning, electricity, caustic chemicals or friction.
Reid Hanson, DVM (Professor of Surgery, College of Veterinary Medicine, Auburn University, Auburn, AL), has treated a number of burn injuries in horses and has written chapters on equine burn injuries for books on medical treatments, discussing the various types and degrees of burns and how they are treated.
“Fortunately, most of the burns we see in horses are first degree burns,” he says. These are similar to sunburn; only the top layers of skin are affected, and they can heal fairly well in a short time, with very little treatment. Prognosis is excellent unless there is ocular or respiratory involvement.
Second degree burns are more serious since they damage some or all of the deeper layers of skin. “These burns are usually painful because the tactile and pain receptors remain intact. However, they typically are not life threatening and are similar to superficial burns but develop vesicles and blisters. These blisters should be left intact for the first 24-36 hours following their formation because the blister fluid provides protection from infection. The intact blister is also less painful than the denuded, exposed surface if the blister breaks,” he explains.
“It’s actually a good sign if the horse has pain in the burned area because this tells you that the burn is not too deep,” he says. This means the nerves have not been destroyed (as they would be in a deeper 3rd degree burn, in which all the skin is gone).
“After 24-36 hours (or even as much as 48 hours in some cases), we typically partially excise the blister and apply an anti-microbial dressing to the wound. This allows the eschar to form, which is collagen tissue, like a scab. Up until about 10 years ago, people thought they should remove scabs from a wound, but now we’ve learned that a scab is very good for protecting the wound,” says Hanson.
TREATING A SERIOUS BURN
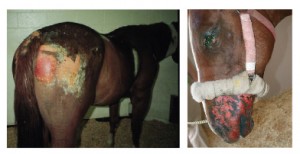 “Third degree burns are the ones that are potentially life-threatening, and the horse must be treated for shock and/or respiratory distress as a first priority. Even though the burns look terrible, what will immediately kill the horse is either life-threatening shock associated with the burn, and/or respiratory distress—which is usually associated with smoke inhalation.” The resultant swelling in the air passages may close off the airways and the horse suffocates.
“Third degree burns are the ones that are potentially life-threatening, and the horse must be treated for shock and/or respiratory distress as a first priority. Even though the burns look terrible, what will immediately kill the horse is either life-threatening shock associated with the burn, and/or respiratory distress—which is usually associated with smoke inhalation.” The resultant swelling in the air passages may close off the airways and the horse suffocates.
A third degree burn goes clear through the dermis (the bottom layer of the skin) into deeper subcutaneous tissues. “This leads to formation of a primary collagenous structure, the eschar, which is almost like a bandage itself. We don’t recommend removal of this eschar. Open wound treatments for extensive burns in horses are not practical, unlike what they do in people—because there’s more likelihood of environmental contamination and massive loss of fluids and body heat due to exposure of all that unprotected tissue,” he explains.
“The most effective and practical therapy for 3rd degree burns in horses is to leave the eschar intact, with 2 to 3-times-a-day application of anti-bacterial agents directly onto the wound. We clip the surrounding hair and debride (remove) the dead, burned tissues. If we are at the scene immediately after the horse is burned, we cool the burn with ice or a cold water bath, and do a lot of lavage over the area with a weak, sterile chlorhexadine solution. This is what a person can do in the first hours, to cool the skin. But too much water applied to the skin will actually do more harm than good–by increasing the formation of edema in the skin” says Hanson.
“After we’ve debrided the tissue and clipped the hair, and have figured out approximately where the burn is, we apply a water-based antibiotic ointment very liberally over the affected areas to prevent heat and moisture loss and protect the eschar. This will also help prevent bacterial invasion, infection of the wound, and potential septicemia of the patient,” he says. As time goes on, these applications also help loosen any remaining necrotic tissue and debris.
“This is a slow method of continuing debridement, allowing removal of all the necrotic tissue, and thereby preventing possible removal of healthy germinal (growing) layers by mistake,” he explains. The eschar is allowed to remain intact as a natural bandage until it is ready to slough off on its own.
You can’t prevent bacteria from getting onto a large wound, so it should be cleansed 2 to 3 times a day, applying the topical antibiotic ointment after each cleaning. “We usually use silver sulfadiazine. We don’t use occlusive dressings (closed, protective) like those used on people. We don’t use wet dressings and wrap them up with antibiotics. Occlusive dressings create a closed wound environment which might encourage bacteria to proliferate and delay healing,” explains Hanson.
“Sometimes we use a sheet soaked in chlorhexadine and drape it over the top line of the horse to protect burned areas over the back, but we don’t do that very often—mainly just at the beginning, to see which layers are intact and which ones are not. That moisture, in the first 12 hours, helps us identify which tissues need to come off right away,” he says.
“The Silvadine cream can be applied as a ‘bandage’ anywhere over the body. We don’t use systemic antibiotics very much because they don’t favorably influence wound healing; there is not enough blood supply to those burned tissues. All you do by giving antibiotics is just promote resistant organisms moving in,” he says.
DEALING WITH SHOCK
Immediately after the burn, the important thing is to prevent or deal with shock. “If a 3rd degree burn exceeds 15 to 20% of the body surface area, the horse will likely need intravenous fluid therapy. We don’t use really large volumes of lactated ringers IV therapy because of the possibility of over-hydrating the horse,” says Hanson. This might increase damage to the lungs, if they’ve suffered from heat or smoke inhalation. If there’s very much edema in the lungs the horse will have serious problems and be more prone to pneumonia.
“We use about 20 liters of fluid, maximum, in an adult horse. We also give Banamine to reduce pain and inflammation and we use Pentoxifylline to help with circulation of blood through the vessels. We carefully and continually monitor the horse’s hydration status, lung sounds, and cardiovascular status,” says Hanson.
“Depending on the horse and the amount of hypoprotenemia (low protein level) that develops, we may give 10 to 20 liters of plasma. In addition, we probably will give DMSO during the first 24 hours, to decrease inflammation and pulmonary edema, pulling the fluid out of the lungs. If the veterinarian suspects that pulmonary edema is present, and it is unresponsive to DMSO treatment, dexamethasone might be given—just once.”
RESPIRATORY DAMAGE
If respiratory signs or smoke inhalation is suspected (and most burns on the face will be a clue that the horse could have smoke or heat inhalation injury), the horse is usually put on systemic antibiotics to treat the lungs. “Unlike burned skin, the lungs still have a good blood supply that can carry the antibiotic to the damaged areas,” he says.
“We usually put these horses on intramuscular injections of penicillin if they have an uninjured area of muscle where we can inject it. This can help deal with contaminants that got into the airway, associated with the smoke. With smoke, there is soot—carbon—and it can easily get into the lungs during the fire. The body then has to eliminate all that carbon and the penicillin helps keep the horse from getting secondary bacterial infections. If respiratory signs deteriorate—if the respiratory rate increases, or the horse is coughing or can’t ventilate very well—then some lung fluid should be aspirated (trans-tracheal aspirate) to do a culture and sensitivity test to determine what other antibiotic might be needed,” says Hanson.
If there is smoke inhalation and the airways begin to swell shut after the fire, a tracheotomy may be required, so the horse can continue breathing. “We only do this if we anticipate there will be some kind of obstruction. We generally do an endoscopy of the trachea after a burn injury, for prognostic purposes, because there may be a lot of sloughing of the mucosa inside the airway. We try to aspirate that sloughed mucosa, but the aspiration procedure should last no longer than 15 second intervals because when you are aspirating material out of the trachea you are also aspirating oxygen out of it as well, making it harder for the horse to breathe,” he says.
“We may give the horse supplemental humidified oxygen through an intranasal catheter. We may (or may not, depending on the horse) nebulize with albuterol, amakacin or acetylecysteine every 6 hours to help with antibacterial protection and to help slough the necrotic tissue. Often we’ll give systemic antioxidant therapy such as oral vitamin E and vitamin C. We may rinse the mouth out every 4 hours with a .05% chlorhexadine solution.”
DAMAGE TO EYES
With many extensive burns, there may also be damage to the eyes. “We check for corneal ulcerations and eyelid burns. If the lids are swollen we apply an ophthalmic ointment to the cornea every 6 hours. We also check twice a day for any evidence of further corneal ulceration. If the cornea is damaged, we very carefully debride the necrotic cornea after the horse is tranquilized, and while using a topical anesthetic. We apply a topical antibiotic and atropine. We do not normally use steroids in the eye because it would delay healing,” says Hanson.
“Occasionally a third eyelid flap may be needed to protect the cornea from severe trauma and damage (as from a necrotic eyelid). Then we can use silver sulfadiazine around the eye, but we need to be careful not to use chlorhexadine in or around the eye.”
NUTRITIONAL NEEDS
“As the horse is recovering from the burn—after we’ve gotten him through the acute things that could kill him, such as smoke inhalation and shock—we need to keep him nutritionally intact,” says Hanson. There’s a lot of healing to accomplish, and this takes more nutrients, to rebuild damaged tissues.
Metabolic rate increases in proportion to the size of the thermal injury, especially if it exceeds 10% of the total body surface area. This increased metabolism causes a rise in core body temperature, and also results in increased oxygen consumption and protein/glucose utilization. “Caloric expenditure and protein breakdown are greater in bury injuries than in any other physiologic stress state. In horses with burns greater than 30% of the body surface, energy expenditure doubles,” he explains.
“Some of the typical things we’ll do to keep the horse from losing weight are to gradually increase the grain and add fat to the diet in the form of vegetable oil, such as 4 to 8 ounces of vegetable oil, and offer free-choice alfalfa hay to increase the caloric intake. Occasionally we’ll use an anabolic steroid to increase the horse’s anabolic status,” says Hanson.
“If smoke inhalation has occurred, or there are burns around the face or scalding of the skin, this means the horse probably has damage to the mucosa in the mouth and the upper airways. In these instances we will soak the hay with water to make it easier to eat and less abrasive to the damaged mouth tissues. We feed the horse on the ground, to encourage drainage from the airways.”
COMPLICATIONS
“Horses may get various types of skin infections following a burn injury. This is why we use silver sulfadiazine to cover the raw areas as they heal, because it is affective against gram negative organisms such as pseudomonas, and has an antifungal activity as well. People often ask about using Aloe Vera but it is more effective after an immediate burn. It has antiprostaglandin and anti-thromboxane properties, which relieves the pain and decreases inflammation. It also has some antibacterial and antifungal activity,” says Hanson.
Often the veterinarian and owner’s efforts can get the horse through the most immediate dangers—shock, smoke inhalation, initial wound care—and then a month or two down the road the horse becomes very itchy. He starts rubbing the healing areas, or chewing on them, and can destroy any progress that’s been made.
The owner needs to be monitoring the horse closely, and very aware of what’s happening. If the horse starts rubbing the burned areas, he may need to be cross-tied and sedated. Antihistamines may be affective in some cases, and Reserpine may be helpful in decreasing the urge to scratch,” he says.
Once the skin heals it may be depigmented, and thus more susceptible to sunburn. If certain areas suffered 3rd degree burns that had to be grafted, the new skin will also be thinner and more fragile (being just the top layers taken from a donor site) and won’t normally have oil glands, sweat glands or hair follicles.
THERAPY AND TREATMENT AFTER THE INJURY
Most of the work involved in the continuing recovery of a burned horse will fall upon the owner. When the owner is doing the treatments it’s time consuming and requires steady commitment, but will be less expensive than having the horse in a hospital facility or treated by a veterinarian. The owner needs to understand that many horses can survive and have a good life—and some will recover enough to go back to normal work. Not every seriously burned horse must be euthanized. But the decision to treat and work with that horse takes major commitment.
“We can get a lot of horses through burn injuries, but it takes time and dedication on the part of the owner,” says Hanson.
Click here to read the complete article